Fiji has the biggest health burdens from diabetes in the world and it continues to rise, despite the country’s small population which should be a concern for everyone.
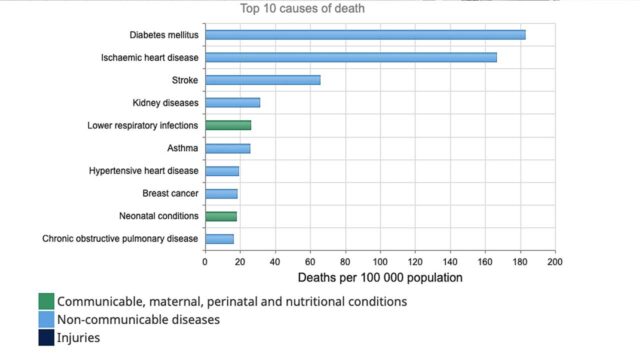
Diabetes is the number 1 killer of Fijians. It is the cause of death for nearly 183 out of every 100,000 people in the country, according to latest data for both sexes and all ages from the World Health Organisation, which is for 2019.
This death rate is even higher at 260.75 per 100,000 people, using age-standardized data from the Global Burden of Disease Study 2019 (Institute of Health Metrics and Evaluation.) This figure has nearly doubled in absolute terms from 162.61 in 1990.
These make Fiji the country with the highest death rate from diabetes.
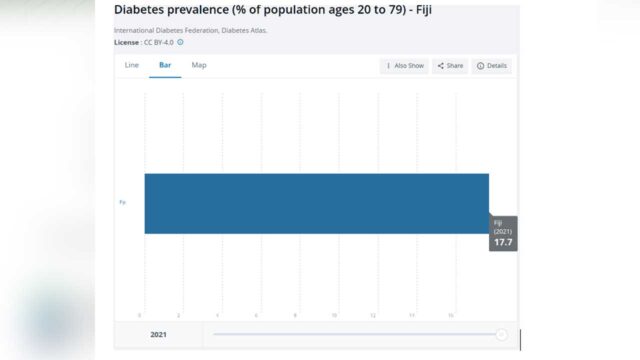
Moreover, Fiji has highest prevalence rates of diabetes in the world. It stands at 17.7% when the global average is 9.8%, going by International Diabetes Foundation and World Bank figures.
Diabetes is among the four main chronic illnesses, or non-communicable diseases, that kill nearly three-fourths of people in the world today.
The toll of non-communicable diseases (NCDs), as these chronic illnesses are called, was also clearly seen during the COVID-19 pandemic. Having morbidities and chronic illnesses – mainly NCDs like cardiovascular diseases, cancers, chronic respiratory diseases and diabetes, increased the risk of severity of COVID-19 for patients.
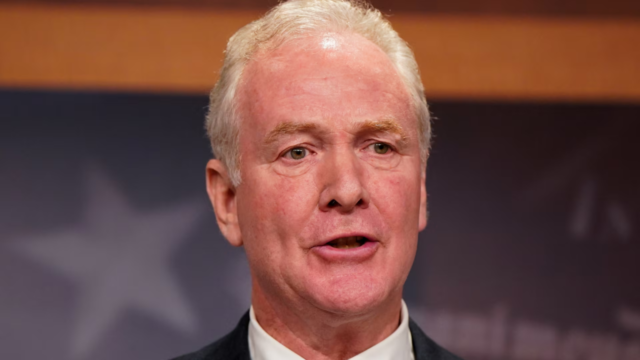
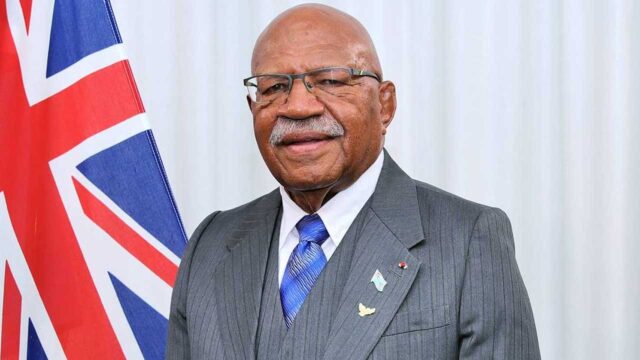
Health Minister Dr Atonio Lalabalavu says in 2020, a year dominated by almost nothing but COVID-19 headlines, Fiji lost an estimated 5,700 Fijians due to NCD-related causes.
These lives were ended too soon by quiet killers like diabetes, stroke, heart disease, and others.
While NCDs are deadly on their own –– COVID-19 turned them into more efficient killers. NCDs and other comorbidities also complicated the Ministry’s ability to precisely determine the causes of death.
Dr Lalabalavu believes that overconsumption of sugar, sweets, and drinks can be linked directly to crippling levels of non-communicable diseases.
The Health Minister believes that this all goes to show how and why the perception of health priorities needs to change.
He adds this is a societal problem that affects every community in Fiji, and saving lives depends on actions from all of us.
He adds the risk factors for NCDs in Fiji are significant and include the high prevalence of overweight and elevated blood sugar and blood pressure levels in our communities, the insufficient daily consumption of healthy food options in fruit and vegetables and the presence of a significant percentage of daily smokers.
Dr Lalabalavu says health statistics show that over 80 per cent of Fiji’s annual mortality is attributed to NCDs, with diabetes, heart disease, kidney diseases and stroke as the top four contributors to death statistics.
The Minister says this trend affects not only the elderly but also younger Fijians in their 20s and 30s
“The burden of NCDs transcends health implications, posing a significant barrier to development and economic growth. The intersection between national policies on development, trade, social protection, international cooperation, to name a few, and population health needs closure, scrutiny, and readjustments towards protecting the health of our people.”
The Ministry has noted a significant shift from our traditional staples, vegetables, and fruits to a high dependence on processed and ultra-processed foods that are high in unhealthy fat, sugar, and salt.
The traditional Fijian food includes Rice, sweet potatoes, taro (a tropical root vegetable), coconuts, cassava (a starchy shrub), breadfruit, and of course fish.
Dr Lalabalavu believes that there has been a shift in the traditional eating habits of Fijians towards a more Westernized or processed food-oriented diet, which could be one of the contributing factors to the rising numbers of NCDs.
Traditional foods are rich in vitamins, minerals, antioxidants, and dietary fiber, contributing to overall health and well-being. Moreover, traditional diets have been associated with reduced risks of chronic diseases, such as heart disease, diabetes, and obesity.
Some of the unhealthy choices that Fijians make is fried chicken, noodles, , soft drinks, fatty, sweet, savory, or salty packaged snacks, biscuits (cookies), ice creams and frozen desserts, chocolates, candies, and confectionery in general, soda, and other carbonated and sugar-sweetened beverages, including ‘energy’ and sports drinks.
He adds that while traditional foods are highly valued in most urban families, they are now mainly consumed at special events and family gatherings, with most meals instead being based on rice, bread, and canned food.
Fijians believe that takeaways and packaged food items is an easy and affordable option in the urban centres due to the fast paced and busy lifestyle.
Meleki from Navua believes that living alone is one factor which contributes to the unhealthy diet for him as he opts to order fast-food which is convenient and easy.
“Given that I leave alone , I don’t actually cook on a daily basis, most of the time I just order takeout’s which is usually, McDonalds, fried chicken or pizza. It is an easier option for me.”
Shital from Suva believes that her unhealthy diet is a way to cope with negative sentiments such as stress, anxiety, and depression.
“Whenever I am sad, angry or depressed I always eat sweet food and drink carbonated drinks. I know it is unhealthy but it is like a rewarding choice for me.”
Vandhana Kumar from Nadi says that urbanisation had led to her moving away from producing and cooking her own food and turn to prepared foods that are often high in sugar, salt and fat.
“When I was living in the village I always had fresh food which we harvested from our farms , but when I moved to Nadi my choices changed because I started relaying more on prepared food.”
Meanwhile, a worrying trend of undernutrition, overweight, and micronutrient deficiencies is impacting Fiji’s youth, putting them at increased risk of developing non-communicable diseases like diabetes and heart disease.
UNICEF Representative to the Pacific Jonathan Veitch highlighted the “triple burden”, stating that more than a third of older children and adolescents are overweight or obese.
“You’ve got extremely high rates of non-communicable diseases that are causing early death and mortality for many, many people. And it’s completely preventable. And the way to prevent it is to make sure that everyone is educated, everybody understands that, and that we promote healthy living. And this requires a whole-government approach because it starts well, even before birth. But at birth, mothers need to be given the opportunity to breastfeed their children, because breastfeeding is the best food for a baby in the first six months.”
Veitch emphasized that the consumption of unhealthy diet needs to be addressed which is affected by a lot of different factors.
“There are lots of different reasons. One is that it’s tasty, and if you put a lot of sugar in something or a lot of sodium or other products in something, it tastes good, and you get kind of addicted to the sugar. You can get addicted to those things at a very young age. That’s one. The other one is peer pressure. They see the other kids eating those things—biscuits and snacks—that are unhealthy, and they want to copy their peers or their brothers and sisters. The other is price. That the prices are incorrect. It shouldn’t be the case that the unhealthy choice is cheaper than the healthy choice. So we need to reverse that. And then perhaps we’ve moved away from the traditional production of homegrown, healthy food.”
On the other hand, the tradition in rural and maritime areas has seen Fijians produce their own fruits and vegetables to maintain a healthy diet.
Meanwhile, recognizing the critical role played by lifestyle choices in shaping the health of Fijians, the ministry is set to transform its strategies, placing an emphasis on community engagement and preventative measures.
Dr Lalabalavu says the ministry’s approach extends beyond the pre-birth phase, extending up to the first 1000 days of a child’s life, a crucial period identified for laying the foundation of lifelong habits.
Lifestyle change is difficult to address because it’s something that, to change your lifestyle, you need to change certain ways of living, ways of thinking, and ways of doing things, and governments as they are. I believe you’ve just put into place an early childhood development policy. This will be looked into not only in the pre-birth phase but also up until the first probably 1000 days of their life. And again, it goes back to how we develop our lifestyle in the early stages.
However, he believes that an inter-ministerial and whole-of-society approach is needed to tackle the issue.
“We’re still seeing the numbers rise. So it goes back to lifestyle changes because non-communicable diseases and lifestyle diseases not only look after but also treat and prevent NCDs. It’s a challenging one in the sense that if the Ministry of Health takes on the sole responsibility of doing this, we will not be able to achieve the outcome. It has to be probably the engagement of everyone inter-ministerial. All communities have to be involved.”
Experts believe that this comprehensive approach will not only contribute to individual lifestyle changes but also have a broader impact on societal norms and values.
There are no latest statistics yet for recent years, but health ministry goes by the projections based on current rates, which highlights that the numbers continue to rise in the prevalence of diabetes including type 1 in children, overweight and obesity, hypertension, cancers (current and emerging), food allergies, anemia, and amputations.
The Healthy Workplace screening conducted in 2022 for over 3400 employees working in the public and private sectors showed that:
• 40.8 percent of employees had a cardiovascular risk;
• 98.1 percent of employees had NCD risk;
• 50 percent of the employees were obese;
• 32 percent had Hypertension with 4.4 percent had severe Hypertension;
• 18.2 percent had borderline random blood sugars and 5.5 percent showing high blood sugars levels.
According to the Ministry diet is the single leading risk factor to death. The other risk factors are physical inactivity, alcohol, tobacco, drugs and substances and stress.
There is a general tendency to also consume unhealthy sugar sweetened beverages and add sugar to beverages such as tea, coffee and other beverages.
The 2002 STEPS Survey results showed that 16 percent of adults aged from 24 to 64 had diabetes. According to MoH 2009 Annual Report, patients at their reproductive age (15 to 64 years) are 80.7 percent of neoplasm cases, 73.7 percent of endocrine, nutritional and metabolic disease cases, and 63.7 percent of diseases of circulatory system cases.
According to 2007 census, 5,888 (1% of people aged 15 or more) were disabled. And around 70% to 90% with disabilities were caused by above-
According to 2007 census, 5,888 (1% of people aged 15 or more) were disabled. And around 70% to 90% with disabilities were caused by above-knee amputation (AKA). The number of disabled has increased from 3,117 in 1996. As shown in Figure below, more than 600 amputations occurred annually.
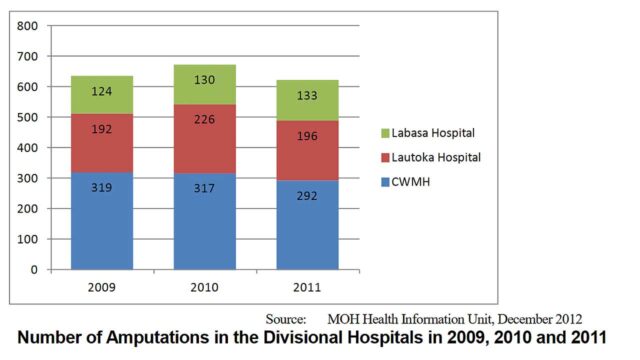
According to health officials, there is one amputation every twelve hours and about 40 percent of all the surgery done in Fiji is for amputation.
The link between diabetes and amputations is primarily due to a condition called diabetic neuropathy and peripheral vascular disease, both of which are complications of diabetes. Diabetes significantly increases the risk of developing cardiovascular diseases such as heart attacks, stroke, and peripheral artery disease. High blood sugar levels can damage blood vessels and lead to atherosclerosis, increasing the likelihood of heart and vascular complications. It is also one of the leading causes of chronic kidney disease (CKD).
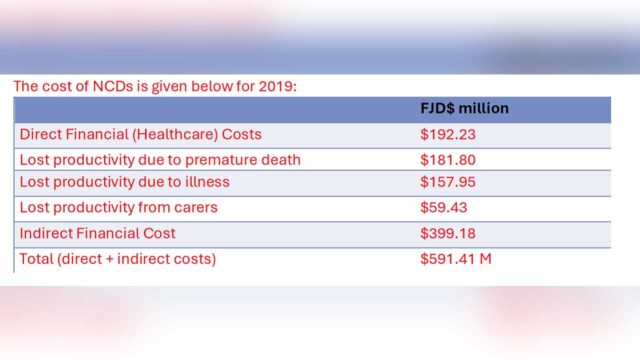
Currently, diabetes and obesity-related illnesses are the leading causes of death and disability in Fiji, with health care costs recorded at $591 million in 2019 .
According to National Nutrition Survey in 2015:
• Anemia – around 63 percent of Children under five, 45 percent of children 5-14 years and 43 percent of children 15-17 years
• Overweight – around 5 percent of children under five, 7 percent of children 5-14 years and 8 percent of children 15-17 years
Meanwhile, In Fiji’s rural and maritime communities, a health option is taking root as Fijians rally to maintain balanced diets and curb the rising tide of non-communicable diseases. Embracing a holistic approach to wellness, residents of the maritime islands are turning to local agriculture to cultivate fresh produce and promote healthier lifestyles.
Fiji’s maritime islands, with their fertile soil and favorable climate, have become hubs of agricultural innovation. Local farmers, equipped with traditional knowledge and modern techniques, are cultivating an array of fruits and vegetables like watermelon, mango, cucumber, cabbage,guava,pineapple,beans and cassava ensuring a diverse and accessible selection for their communities
Sovita Turagabeci from Gau Island a passionate farmer, expressed the community’s determination to prioritize health.
“We understand that our strength lies in the health of each member of our community. By prioritizing health, we not only ensure the longevity of our people but also create a foundation for a vibrant and resilient society.”
Another farmer Tuta Pareti from Vanuabalavu Lau believes that their tight bonds in the island foster a shared commitment to well-being.
“We on the island work together and help each other on the farm so that we are able to produce for our whole village and maintain food security because here we do not depend on processed food.”
Village headman Luke Ceva from Navosa says the commitment to healthier eating is not only improving individual well-being but is also seen as a collective effort to combat non-communicable diseases, such as diabetes and hypertension, which have been on the rise in Fiji.
“I think we in the village have the advantage because we have our own land that we can cultivate and produce healthy fruits and vegetables which also helps us to stay fit and provide for other Fijians and supply fresh produce to the markets. However those living in the urban centres don’t have all this therefore they go for cheaper options.”
Recognizing the importance of a balanced diet rich in fruits and vegetables Ceva says they have dedicated themselves to growing fresh, nutrient-packed produce.
“We believe that what we eat directly impacts our well-being. By growing our own fruits and vegetables, we are not only ensuring a steady supply of fresh and nutritious food but also reducing our reliance on processed and unhealthy options”
Jone Vakaloloma from Nawaikama , Gau says they have embraced the idea that our health starts with what we put on our plates.
“Growing our own produce allows us to control the quality of our food, ensuring that our community has access to the freshest and healthiest options.”
“This story was produced under the “Communicating NCDs” Media Fellowship by Probe Media Foundation Inc. (PMFI), Reporting ASEAN (RA), and World Health Organization (WHO) Western Pacific Regional Office. The views and opinions expressed in this piece are not necessarily those of PMFI, RA, and WHO.”
Stream the best of Fiji on VITI+. Anytime. Anywhere.

 Kreetika Kumar
Kreetika Kumar